Connect With Us
Blog
Items filtered by date: May 2025
Linking Foot Pain and Arthritis

Foot pain is often linked to various forms of arthritis that affect the joints, soft tissues, and structure of the feet, toes, and ankles. Osteoarthritis can cause the cartilage in foot joints to wear down over time, leading to stiffness, pain, and changes in walking mechanics. Rheumatoid arthritis, an autoimmune condition, frequently affects both feet symmetrically and may lead to joint deformities like hammertoes or claw toes. Psoriatic arthritis may cause inflammation in tendons and ligaments, contributing to conditions like plantar fasciitis and Achilles tendonitis. Gout often causes sudden, intense pain in the big toe or ankle due to the buildup of uric acid crystals. Lupus-related arthritis can lead to joint pain, nerve damage, and poor circulation in the feet. A podiatrist can provide an accurate diagnosis and recommend treatment, which may include medication, custom orthotics, or surgery. If you are experiencing foot pain, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Melissa C. Verde, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a joint disorder that involves the inflammation of different joints in your body, such as those in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. In addition to this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
- Exercises that stretch the foot can prevent further pain and injury and increase mobility
- Most of the pain can be alleviated with anti-inflammatory drugs, heat, and topical medications
- Massages can help temporarily alleviate pain.
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions please feel free to contact our office located in Longwood, FL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Causes and Symptoms of Plantar Fasciitis
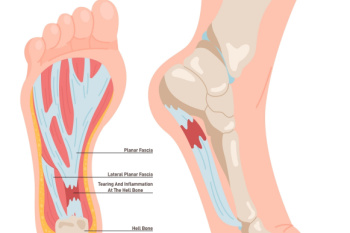
Plantar fasciitis occurs when the band of tissue that runs along the bottom of the foot, called the plantar fascia, becomes irritated or inflamed. This ligament supports the arch and absorbs pressure during walking. Repeated strain from activities like running, long periods of standing, or wearing shoes that lack proper support can lead to small tears where the fascia connects to the heel bone. Symptoms of plantar fasciitis often include sharp pain in the heel, especially with the first steps in the morning or after sitting for long periods. The pain may recede with movement but often returns later in the day. A podiatrist can diagnose plantar fasciitis by examining the foot and reviewing activity history. Treatment options include prescribed orthotics, anti-inflammatory medication, night splints, or, in some cases, corticosteroid injections. Surgery may be considered if other options fail. If you have pain on the bottom of your foot, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Melissa C. Verde, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions, please feel free to contact our office located in Longwood, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Exercises After a Sprain

Recovering from a sprained ankle involves a gradual process of restoring motion, building strength, and improving balance to protect the joint from future injury. A podiatrist may recommend ankle exercises, starting with light range-of-motion exercises like flexing the foot upward and downward or tracing the alphabet with the toes within the first 48 hours to encourage flexibility. Strengthening exercises are added as healing progresses, including ankle eversion and inversion movements. Ankle eversion strengthens the muscles on the outer side of the ankle by turning the foot outward against resistance, while ankle inversion works the muscles on the inner side by turning the foot inward. These exercises help stabilize the ankle and prevent chronic sprains. By the third or fourth week, a patient may perform standing stretches to loosen tight calf muscles and practice toe rises to build endurance. Moving too quickly can place unnecessary stress on healing tissues, so guidance from a foot specialist is important. If you have sprained your ankle, it is suggested that you schedule an appointment with a podiatrist for initial treatment as well as a recovery plan.
Ankle sprains are common but need immediate attention. If you need your feet checked, contact Melissa C. Verde, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains take place when the ligaments in your ankle are torn or stretched beyond their limits. There are multiple ways that the ankle can become injured, including twisting or rolling over onto your ankle, putting undue stress on it, or causing trauma to the ankle itself.
What Are the Symptoms?
- Mild to moderate bruising
- Limited mobility
- Swelling
- Discoloration of the skin (depending on severity)
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
Treatment of a sprain depends on the severity. Many times, people are told to rest and remain off their feet completely, while others are given an air cast. If the sprain is very severe, surgery may be required.
If you have suffered an ankle sprain previously, you may want to consider additional support such as a brace and regular exercises to strengthen the ankle.
If you have any questions please feel free to contact our office located in Longwood, FL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Facts About Cracked Heels

Cracked heels, also known as heel fissures, occur when the skin on the heels becomes dry, thickened, and eventually splits. This condition often results from a lack of moisture and pressure on the fat pad under the heel, causing the skin to expand and crack. Symptoms of cracked heels include dry, rough skin, visible splits or fissures, pain while walking, and, in severe cases, bleeding or infection. Risk factors for developing cracked heels include prolonged standing, walking barefoot, wearing open-backed shoes, obesity, and certain skin conditions like eczema or psoriasis. Additionally, environmental factors such as cold weather and low humidity can also contribute to this condition. If you have developed painful cracked heels, it is suggested that you consult a podiatrist who can offer effective relief remedies, which may include prescribed medication.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Melissa C. Verde, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our office located in Longwood, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
